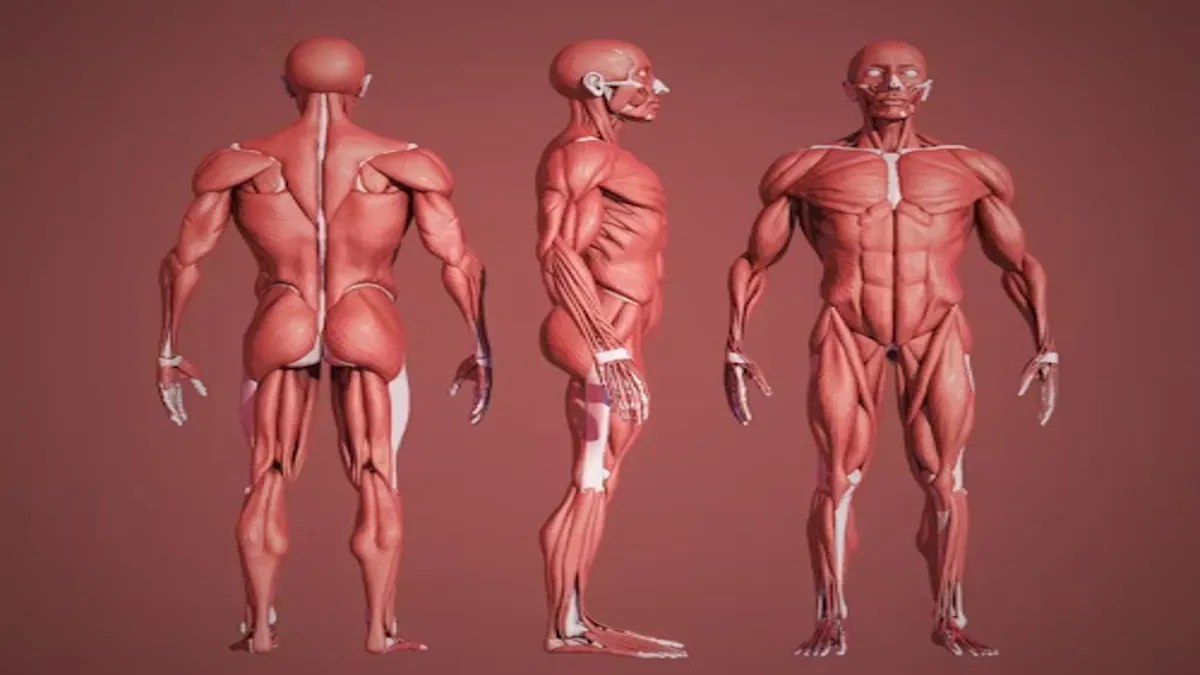
Inomyalgia has emerged as a term people increasingly use to describe persistent muscle pain, stiffness, and exhaustion that extend far beyond normal soreness, often affecting daily routines and emotional well-being. Within the first 100 words: inomyalgia signifies chronic muscle discomfort that lingers for months or years, disrupting movement, sleep, cognition, and mood, and resisting traditional explanations offered by established diagnoses. While not formally recognized in medical classifications, the term has grown in visibility because it captures a pattern of suffering that many feel has remained unacknowledged and undefined. As discussions intensify, inomyalgia represents both a descriptive label and a social signal: patients are telling clinicians, researchers, and communities that something vital is missing from current approaches to chronic muscle pain. This article examines inomyalgia as a lived experience, conceptual framework, and emerging conversation about the nature of pain, validation, and the need for more inclusive care.
Understanding the Term and Its Origins
The term inomyalgia draws on Greek linguistic roots combining elements meaning “muscle fibers” and “pain,” creating a phrase that translates roughly to “pain within muscle tissues.” Within patient communities, it serves as shorthand for chronic muscle discomfort that lacks clear clinical classification. Unlike formally acknowledged conditions, inomyalgia does not appear in standardized diagnostic frameworks, leaving individuals without structured guidelines for identification or treatment. In various patient-driven descriptions, it conveys a constellation of symptoms discomfort, stiffness, tension, fatigue, and reduced physical resilience that collectively shape daily function. Because these experiences rarely fit neatly into established medical categories, the terminology serves as both a descriptor and a form of self-advocacy. Patients use it to articulate suffering that otherwise receives fragmented explanations or, at times, dismissal. Thus, the rise of inomyalgia underscores a broader tension between lived experiences and the limitations of conventional diagnostic language.
Symptom Patterns and Overlapping Experiences
Individuals who use the term inomyalgia typically describe a set of recurring symptoms that interfere with physical performance, rest, and concentration. These include long-lasting muscle soreness; morning stiffness; heightened sensitivity when pressure is applied; fatigue that persists despite adequate rest; and cognitive difficulty that affects focus or memory. The picture that emerges resembles — but does not fully duplicate — profiles found in better-known chronic pain conditions. The similarity often causes confusion: symptoms overlap with those associated with complex systemic disorders, yet patients feel their experiences remain more specifically muscular and less reliant on neurological or multisystem interpretation. This distinction, though subtle, matters deeply to those seeking a term that reflects their embodied reality rather than a diagnostic model they feel doesn’t capture their core discomfort. Inomyalgia thus becomes a symbolic answer to the gap between symptom clusters and existing medical definitions.
The Emotional and Social Dimensions of Naming Pain
For many, adopting the term inomyalgia is not simply an attempt to classify symptoms; it is a response to emotional, social, and clinical invisibility. Chronic muscle pain shapes mobility, relationships, employment, and psychological health, creating cycles of frustration and self-doubt. Without diagnostic recognition, individuals often experience dismissal, misunderstanding, or accusations of exaggeration. A named condition — even an unofficial one — offers language for self-expression, validation, and community formation. It transforms isolated discomfort into a shared vocabulary that invites empathy and solidarity. For some, the term provides a sense of legitimacy in clinical encounters, helping convey that their symptoms are neither imagined nor trivial. This human need for acknowledgment explains why inomyalgia has taken root: it represents not only physical pain but also the desire for identity, clarity, and support within an overwhelming landscape of chronic illness.
Comparison Between Inomyalgia and Related Conditions
| Dimension | Inomyalgia (described by patient communities) | Fibromyalgia (established clinical condition) |
|---|---|---|
| Pain Location | Primarily muscular, focused on sore or tense regions | Widespread pain across multiple body areas |
| Recognition | Informal, patient-driven terminology | Formal clinical diagnosis with criteria |
| Associated Symptoms | Stiffness, fatigue, variable tenderness | Sleep disturbance, cognitive symptoms, systemic involvement |
| Diagnostic Process | None standardized; descriptive only | Structured clinical evaluation |
| Perceived Mechanism | Muscle-based discomfort | Altered pain processing, neurological involvement |
This comparison illustrates why some patients gravitate toward the term inomyalgia: it feels closer to their muscle-specific symptoms than broader, multisystem labels.
Treatment Approaches Described by Patient Communities
Management strategies discussed by individuals using the term inomyalgia generally emphasize supportive, non-pharmacologic care due to the absence of official treatment guidelines. These approaches focus on improving muscle resilience, reducing stiffness, and supporting the body’s natural recovery processes. Gentle exercise practices — stretching, walking, yoga, and low-impact strengthening — appear commonly recommended for maintaining flexibility and circulation. Stress-reduction tools such as mindfulness, breathing techniques, and pacing routines help reduce physiological tension that may exacerbate symptoms. Rest and sleep habits receive particular emphasis, as fatigue often amplifies discomfort. Where appropriate, massage, warm compresses, hydration, and gradual activity modification can complement self-care. Because the term lacks clinical definition, individuals often navigate a trial-and-error process to find strategies that offer relief, reflecting broader challenges faced by all chronic pain patients whose symptoms resist straightforward categorization.
Why Recognition Remains Complex
Inomyalgia’s lack of formal recognition highlights structural challenges in chronic pain medicine. Clinical frameworks depend heavily on measurable markers, reproducible patterns, and validated criteria, while patient-defined terms often arise from subjective experience rather than controlled research. This creates friction: patients see the condition as real, lived, and disruptive, while medical systems require evidence that has not yet been established. As a result, individuals using the term inomyalgia find themselves in a liminal space — their pain acknowledged by their own communities but rarely validated in medical settings. This disconnect reveals deeper questions about how pain should be defined, who gets to define it, and how healthcare should respond when suffering falls outside existing categories. Inomyalgia thus symbolizes not only a type of pain, but a broader debate about how society understands and measures human discomfort.
The Need for More Inclusive Frameworks
The emergence of inomyalgia suggests a growing demand for clinical approaches that better account for varied pain experiences. Patients seeking this terminology want more nuanced explanations that distinguish muscular discomfort from broader systemic syndromes. They want care models that combine physical therapy, lifestyle support, and emotional validation rather than relying solely on diagnostic labels. Clinicians, meanwhile, express the need for systematic documentation, clearer symptom mapping, and research that clarifies whether this descriptive term reflects a distinct pattern or a variant of existing chronic pain classifications. Reconciling these perspectives will require collaborative dialogue between patients, researchers, and practitioners — a process that recognizes the legitimacy of lived experience while maintaining scientific rigor. Ultimately, the inomyalgia conversation highlights the importance of empathy, curiosity, and open-minded inquiry in advancing pain science.
Takeaways
- Inomyalgia is a patient-driven term describing chronic muscle pain, stiffness, and fatigue.
- It is not an official medical diagnosis but reflects real, persistent symptoms.
- Individuals use the label for clarity, validation, and community identity.
- Symptoms overlap with recognized chronic pain disorders but feel more muscle-specific.
- Supportive, lifestyle-based management strategies dominate because no formal guidelines exist.
- The term underscores the need for more responsive and inclusive chronic pain frameworks.
Conclusion
Inomyalgia stands at the crossroads of language, suffering, and the human search for understanding. Though unofficial, it expresses something profoundly real: the weight of chronic muscle pain and the yearning for recognition when traditional labels fall short. The experiences described under this term remind us that diagnosis is not merely a clinical exercise but also a social and emotional one. People seek names for their pain not only to categorize symptoms but to be seen, believed, and supported. Whether inomyalgia eventually becomes a clinically defined condition or remains a community-generated descriptor, its existence challenges healthcare systems to listen more deeply to the voices of those who struggle with persistent discomfort. It invites a future where chronic pain — in all its varied forms — is met with compassion, curiosity, and a commitment to understanding what patients are trying to tell us.
FAQs
What does inomyalgia refer to?
It describes long-lasting muscle pain, stiffness, and fatigue as reported by patients seeking a meaningful label for their symptoms.
Is it an official diagnosis?
No. It is a descriptive term used by individuals rather than a medically recognized condition.
How does it differ from fibromyalgia?
Inomyalgia is described as more muscle-focused, while fibromyalgia involves widespread, multisystem pain and formal diagnostic criteria.
What helps manage symptoms?
Gentle movement, rest, stress-reduction techniques, and supportive physical therapies are commonly used approaches.
Can someone with inomyalgia-like symptoms seek medical evaluation?
Yes. Clinical evaluation is essential to rule out other conditions and design appropriate management plans.
REFERENCES
- EpicPlacesss. (n.d.). Inomyalgia: The term, possible meanings, and health relevance. https://epicplacesss.com/inomyalgia-the-term-possible-meanings-and-health-relevance/
- Beziddi. (n.d.). Inomyalgia. https://www.beziddi.com/inomyalgia/
- InternalsUSA. (n.d.). Inomyalgia explained: Chronic muscle pain guide. https://internalsusa.com/inomyalgia-explained-chronic-muscle-pain-guide/
- Scope24. (n.d.). Inomyalgia explored: Navigating the challenges of chronic pain. https://scope24.net/inomyalgia-explored-navigating-the-challenges-of-chronic-pain/
- Merlin Physio. (n.d.). Inomyalgia: Breaking the stigma around chronic pain conditions. https://merlinphysio.com/inomyalgia-breaking-the-stigma-around-chronic-pain-conditions/
- Interior Redoux. (n.d.). Inomyalgia. https://interiorredoux.com/inomyalgia/