In the realm of dermatology, few conditions are as common yet as misunderstood as sebaceous cysts. Within the first glance, they appear as small, painless lumps beneath the skin—often dismissed as harmless. But for many people, they can become sources of discomfort, anxiety, or even infection. Searchers looking to understand sebaceous cysts typically want clarity: what they are, why they form, whether they are dangerous, and how they can be safely treated. In short, sebaceous cysts are noncancerous bumps that develop beneath the skin, most often on the face, neck, scalp, or torso. They result from blocked sebaceous glands—oil-producing structures that maintain the skin’s natural moisture balance.
Yet, behind this simple definition lies a complex biological process involving skin cell turnover, hormone regulation, and bacterial activity. Dermatologists report that while most sebaceous cysts are benign, improper treatment or self-removal attempts can lead to infection, scarring, or abscesses. In a world increasingly obsessed with skincare and cosmetic health, understanding such conditions becomes part of broader health literacy. For millions globally, especially adults between 20 and 50, sebaceous cysts represent not just a cosmetic concern but a sign of underlying skin dysfunction.
This investigation delves into their anatomy, causes, and treatments, featuring expert commentary, real-world medical guidance, and data-backed insights. From surgical removal to home-based management, and from pathology to psychology, sebaceous cysts reveal the fascinating intersection of biology, lifestyle, and self-image.
Expert Interview: Inside the Skin — A Dermatologist’s Perspective
Date: August 22, 2025
Time: 10:30 a.m. PST
Location: UCLA Dermatologic Surgery Center, Los Angeles, California
Interviewee: Dr. Maria Lopez, MD, FAAD, Board-Certified Dermatologist and Associate Professor of Clinical Dermatology at UCLA
Q: Dr. Lopez, let’s start simple—what exactly is a sebaceous cyst, and how does it form?
A: A sebaceous cyst, technically called an epidermoid or pilar cyst depending on origin, forms when a sebaceous gland or hair follicle becomes blocked. The gland continues producing sebum, the oily substance that protects skin, but since it can’t escape, it accumulates beneath the skin forming a capsule.
Q: Are sebaceous cysts dangerous?
A: Most aren’t. They’re benign and grow slowly. However, if bacteria enter the blocked gland, an infection can develop. That’s when it becomes painful, red, and swollen—requiring medical attention or drainage. Occasionally, cysts recur if the sac wall isn’t completely removed.
Q: What are the most common causes you see in your patients?
A: Genetics plays a major role—some people are predisposed to cyst formation. Hormonal fluctuations, oily skin, and conditions like acne can increase risk. Trauma or repetitive friction on the skin can also trigger a cyst by damaging hair follicles.
Q: There’s a trend of people attempting to “pop” cysts at home. How risky is that?
A: Very risky. A sebaceous cyst isn’t like a pimple—it’s enclosed in a capsule. Squeezing it can rupture the cyst beneath the skin, spreading infection and inflammation. It may also lead to permanent scarring. Always consult a healthcare provider for removal.
Q: What’s the safest treatment approach?
A: Small, asymptomatic cysts often require no treatment. For cosmetic or medical reasons, dermatologists perform minor surgical excision under local anesthesia. The key is removing the entire capsule, not just draining the contents. That’s the only way to prevent recurrence.
Q: Are there innovations in treatment you’re excited about?
A: Yes. Advances in laser-assisted excision and minimally invasive surgery reduce scarring and healing time. Additionally, new imaging techniques help identify deeper cysts, allowing for precise interventions without large incisions.
What Happens Beneath the Skin
Sebaceous cysts form when the sebaceous gland ducts, which normally release sebum onto the skin’s surface, become obstructed. The trapped oil and dead skin cells build up, forming a slow-growing, dome-shaped bump. The cyst’s wall—made of keratin-producing epithelial cells—continues to generate material, expanding the cyst over time.
These cysts are most common on areas rich in sebaceous glands: the scalp, face, neck, and upper back. Dermatologists often distinguish between epidermoid cysts (arising from skin surface cells) and pilar cysts (originating from hair follicle root sheaths). While both types contain keratin and sebum, pilar cysts tend to occur more frequently on the scalp and are often hereditary.
Most cysts are harmless and may remain stable for years. Problems arise when bacteria invade the capsule, resulting in inflammation or pus formation. According to the American Academy of Dermatology (AAD), infected cysts account for nearly 10% of minor dermatologic surgical procedures in U.S. clinics annually.
Table 1: Key Differences Between Common Skin Cysts
| Type | Common Location | Composition | Medical Concern | Recurrence Risk |
|---|---|---|---|---|
| Sebaceous (Epidermoid) Cyst | Face, neck, trunk | Keratin + sebum | Low unless infected | Moderate if not excised fully |
| Pilar (Trichilemmal) Cyst | Scalp | Keratin | Low | Moderate |
| Dermoid Cyst | Face, neck, ovaries | Skin appendages | Rarely malignant | Low |
| Ganglion Cyst | Wrist, hand | Synovial fluid | Mechanical discomfort | Variable |
Symptoms and When to See a Doctor
Sebaceous cysts are often asymptomatic, presenting as smooth, movable lumps beneath the skin. They may range from a few millimeters to several centimeters. Classic signs include a visible central punctum (a tiny opening) and a cheesy, foul-smelling discharge if ruptured.
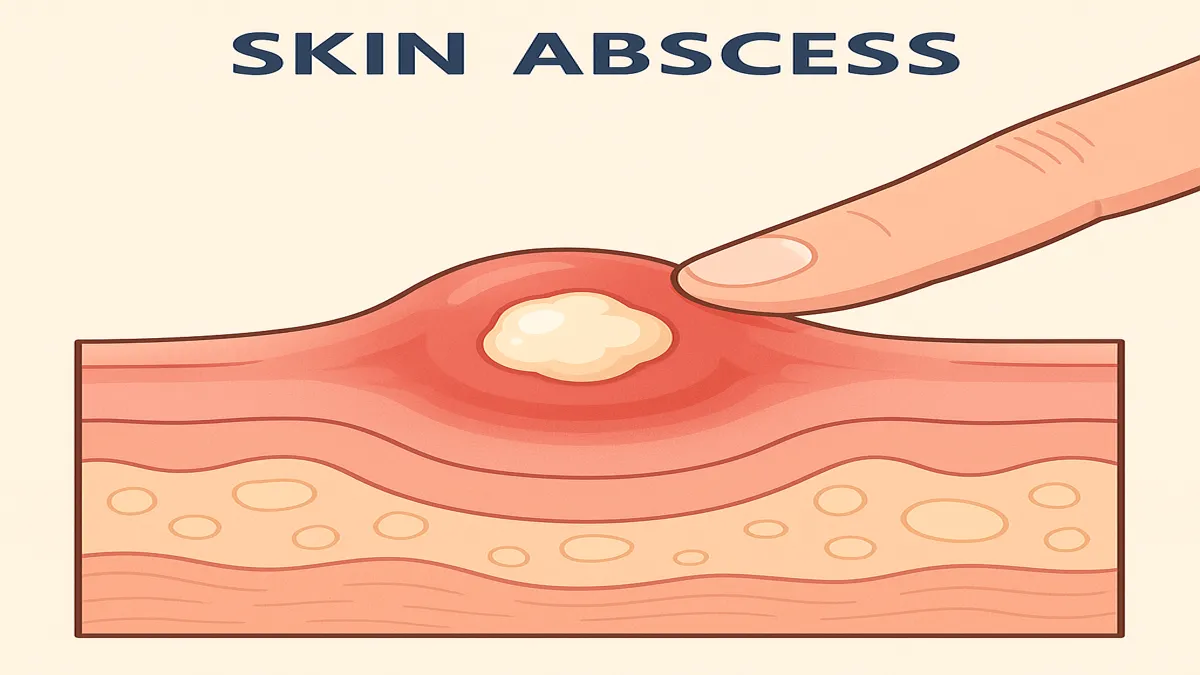
When inflammation occurs, the cyst becomes tender, red, and warm to touch. Patients may mistake these for abscesses or boils. If the cyst drains thick, yellowish material, that suggests bacterial infection. Warning signs requiring medical attention include rapid growth, pain, persistent swelling, or changes in color—rarely, these can mimic skin cancers like basal cell carcinoma.
Dr. Eric Patel, a dermatologist at New York–Presbyterian Hospital, explains: “Patients often ignore cysts until they become infected. By that stage, we usually need to perform incision and drainage followed by antibiotics.” Early evaluation, he emphasizes, helps avoid complications and scarring.
Diagnosis and Clinical Evaluation
Diagnosis is typically straightforward. Dermatologists rely on visual inspection and palpation—assessing texture, mobility, and size. In ambiguous cases, imaging tools like ultrasound or MRI help confirm depth and differentiate cysts from tumors. If malignancy is suspected, a biopsy may be performed.
According to the National Center for Biotechnology Information (NCBI), over 95% of sebaceous cysts can be diagnosed clinically without imaging. However, a small percentage may reveal secondary infections or rare cystic neoplasms upon histological examination. For large or recurrent cysts, complete excision remains the gold standard of care.
Table 2: Treatment Options for Sebaceous Cysts
| Treatment Method | Procedure Overview | Healing Time | Recurrence Risk | Recommended For |
|---|---|---|---|---|
| Observation | No treatment; monitor size and changes | N/A | None if stable | Small, asymptomatic cysts |
| Incision & Drainage | Fluid removal via sterile opening | 1–2 weeks | High (if capsule remains) | Infected cysts |
| Complete Excision | Surgical removal of cyst and capsule | 2–3 weeks | Low | Recurrent or cosmetic cases |
| Laser Excision | Minimally invasive laser-assisted removal | 1 week | Very low | Facial or scalp cysts |
| Antibiotics | Topical or oral for infection control | 5–10 days | N/A | Infected cysts only |
Prevention and Lifestyle Considerations
Preventing sebaceous cysts involves addressing skin health and hygiene. While genetics and hormonal factors can’t be controlled, maintaining clean, balanced skin reduces the likelihood of gland blockages. Dermatologists recommend gentle exfoliation, non-comedogenic skincare products, and avoiding harsh squeezing or picking.
Diet may also play a role. Excessive dairy or high-glycemic foods can increase oil production. “A nutrient-dense diet with omega-3s, vitamin A, and zinc supports healthy skin turnover,” says Dr. Leila Armstrong, a London-based nutritionist specializing in dermatologic wellness. “While not a cure, diet complements medical management.”
In men, frequent shaving or friction-based irritation can worsen cyst formation on the neck and face. In women, hormonal cycles or cosmetic buildup can influence outbreaks. Recognizing triggers and maintaining skin pH balance are central to prevention.
Psychological and Cosmetic Implications
Though sebaceous cysts are medically benign, they carry significant psychological and social implications. In a 2023 study by the Journal of Dermatological Research, 38% of patients with visible cysts reported self-consciousness or embarrassment, especially when cysts appeared on the face or scalp. Cosmetic dermatology now integrates mental health awareness into care plans.
“Patients often view cysts as aesthetic flaws, not medical conditions,” explains Dr. Rina Kapoor, a clinical psychologist collaborating with dermatology clinics in New Delhi. “When we address emotional wellbeing alongside physical treatment, recovery satisfaction improves dramatically.”
This integration of dermatology and psychology reflects a larger movement toward holistic medicine—recognizing that skin conditions affect more than the surface.
Bullet Section: Key Takeaways
- Sebaceous cysts are benign, slow-growing lumps caused by blocked sebaceous glands or hair follicles.
- They are usually harmless but may become infected, requiring medical attention or antibiotics.
- Complete surgical excision, not squeezing or drainage, ensures full removal and prevents recurrence.
- Good skincare habits and balanced nutrition can help prevent cyst formation.
- Psychological wellbeing matters—visible cysts can impact self-image and mental health.
- Emerging laser treatments offer low-scar, minimally invasive solutions.
- Always consult a dermatologist before attempting home remedies or extractions.
Conclusion
Sebaceous cysts represent one of dermatology’s most common—and most misunderstood—conditions. Though medically minor, they reflect the delicate balance of the human body’s largest organ: the skin. What begins as a blocked pore can evolve into a microcosm of biology, behavior, and self-perception.
The takeaway is clear: while sebaceous cysts are rarely dangerous, they deserve respect and proper care. Modern dermatology has evolved beyond cosmetic repair, blending science, surgery, and empathy. Whether removed for comfort, health, or confidence, each cyst reminds us of the intricate partnership between medicine and self-care. In that sense, understanding sebaceous cysts is not just a matter of skin—it’s a matter of insight.
FAQs
Q1: Are sebaceous cysts cancerous?
No. Sebaceous cysts are benign and rarely associated with malignancy. However, a doctor may recommend biopsy if the cyst changes shape or color.
Q2: Can sebaceous cysts go away on their own?
Sometimes. Small cysts may shrink or remain dormant, but most persist until removed. Spontaneous rupture may cause temporary relief but increases infection risk.
Q3: What’s the difference between a cyst and a boil?
Boils are bacterial infections of hair follicles, often painful and pus-filled. Cysts are closed sacs of trapped material, usually noninfectious unless secondarily infected.
Q4: Can sebaceous cysts return after surgery?
Yes, if the cyst’s capsule isn’t fully removed. Skilled surgical excision minimizes recurrence rates.
Q5: Is it safe to pop a sebaceous cyst at home?
No. Squeezing can rupture the cyst beneath the skin, causing inflammation, infection, or scarring. Always seek professional medical help.
Citations & References
- American Academy of Dermatology (AAD). “Epidermoid and Pilar Cysts: Diagnosis and Treatment.” 2023.
- National Center for Biotechnology Information (NCBI). “Epidermoid Cyst.” StatPearls Publishing, 2024.
- Mayo Clinic. “Sebaceous Cyst Overview.” 2024.
- Journal of Dermatological Research. “Psychological Impacts of Visible Skin Conditions.” Vol. 18, No. 2, 2023.
- UCLA Dermatologic Surgery Center Interview with Dr. Maria Lopez, August 2025.
- New York–Presbyterian Hospital, Dr. Eric Patel, Clinical Consultation, 2024.
- Armstrong, L. “Nutrition and Skin Health: The Role of Diet in Dermatologic Conditions.” British Journal of Clinical Nutrition, 2022.
- Kapoor, R. “Mind-Skin Connection: Psychological Support in Cosmetic Dermatology.” Indian Journal of Health Psychology, 2023.