Urobilinogen, though largely invisible in the body’s daily biochemical traffic, carries disproportionate diagnostic weight. Formed within the intestines when bacteria reduce bilirubin, this colorless compound becomes a crossroads where liver function, red blood cell recycling, intestinal microbial activity, and kidney filtration intersect. Most people will never hear of it, yet it quietly influences the color of stool, contributes indirectly to urine’s familiar yellow tint, and signals whether deeper processes inside the body are functioning smoothly or beginning to falter.
Within the first hundred words, the question many readers bring is simple: what does urobilinogen actually tell us about our health? The answer begins with bilirubin, the by-product of red blood cell breakdown. When bilirubin enters the intestines as part of bile, microbes convert it into urobilinogen, some of which continues on to become the pigments in feces, while another portion reenters circulation and is eventually excreted through the kidneys. Thus, any disruption whether from liver inflammation, bile duct blockage, antibiotic-driven microbiome shifts, or accelerated red blood cell destruction can alter urobilinogen levels in predictable ways.
Understanding this compound, therefore, means understanding the deeper choreography of heme metabolism and the constant interplay between organs that depend on one another to keep the body’s internal chemistry in balance.
The Biochemical Pathway: How Urobilinogen Emerges
Bilirubin’s journey begins with the dismantling of old red blood cells, a process carried out chiefly by the spleen, liver, and bone marrow. Once bilirubin arrives at the liver, it undergoes conjugation and is released into the intestine via bile. There, intestinal bacteria reduce it into urobilinogen a fleeting, colorless intermediary.
Most of this urobilinogen will not remain as such for long. Around 80 percent progresses through further chemical changes, oxidizing into pigments responsible for the brown coloration of stool. The remainder is reabsorbed, carried back to the liver, and either recycled into bile or allowed to circulate systemically before being filtered out by the kidneys. This delicate and continuous loop is central to how the body handles the waste products of aging red blood cells.
When the enterohepatic cycle functions normally, urinary urobilinogen remains low but detectable. When it does not, subtle shifts in its levels can point toward important physiological disturbances long before more dramatic symptoms appear.
Why Urobilinogen Matters Clinically
The reason clinicians still pay attention to urobilinogen despite the sophistication of modern biomarkers is its unique position. It reflects multiple processes at once: the production of bilirubin, the liver’s ability to conjugate and excrete it, the open flow of bile into the intestine, and the microbial ecosystem that transforms bilirubin into its downstream compounds.
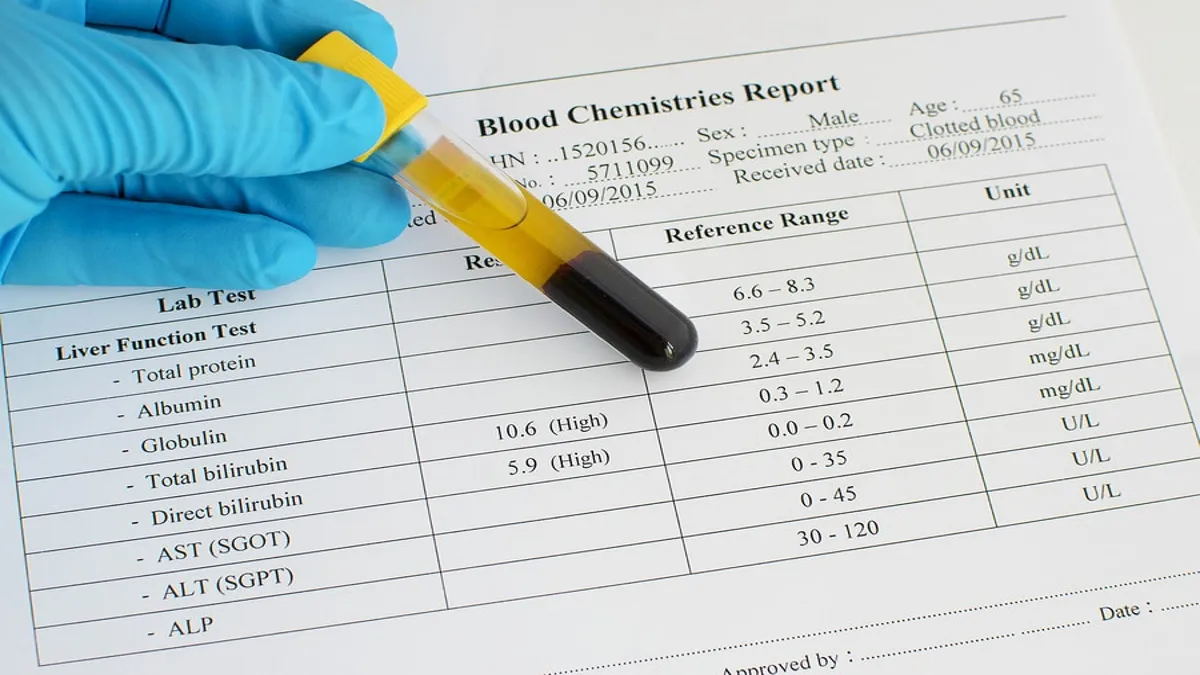
Small amounts of urobilino-gen in the urine are expected. Elevated levels, however, may indicate increased bilirubin production or reduced hepatic clearance. Conversely, extremely low or absent urobilinogen may suggest that bilirubin is not reaching the intestines at all, often due to bile duct obstruction or cholestatic disorders. These shifts do not diagnose a condition outright, but they create a biochemical profile that can guide deeper investigation.
In an era where liver disease is increasingly common and metabolic disorders continue to rise, the quiet information urobilinogen provides remains clinically valuable.
Reading the Signals: Patterns and Interpretations
Typical Diagnostic Patterns Table
| Clinical Scenario | Expected Urobilinogen Level | Physiological Meaning |
|---|---|---|
| Increased red blood cell destruction | Elevated | More bilirubin reaches the intestine, increasing urobilinogen formation |
| Liver inflammation or injury | Elevated or high-normal | Impaired hepatic handling allows more urobilinogen to circulate |
| Bile duct obstruction | Very low or absent | Bilirubin cannot reach the intestine for conversion |
| Major shifts in gut flora | Low | Reduced bacterial reduction of bilirubin |
| Late-stage liver failure | Variable | Early leakage may elevate levels, followed by diminished production |
These patterns illustrate why urobilinogen serves best as part of a broader diagnostic mosaic. It is not a standalone verdict but rather a subtle indicator woven into a larger story of organ interplay.
Three Expert Perspectives
“Urobilinogen offers a window into the intertwined relationship between the liver and the gut — two systems that must cooperate constantly to maintain metabolic balance.”
“Because intestinal bacteria are responsible for its creation, urobilinogen reminds clinicians that the microbiome is not a peripheral actor but a central participant in human physiology.”
“Abnormal levels rarely speak alone. The value of urobilinogen lies in its ability to amplify other clinical signals and reveal the direction in which the underlying pathology is leaning.”
These viewpoints capture a recurring theme: urobilinogen is meaningful not because it stands apart, but because it reflects the integrity of several essential processes at once.
Gut Microbiota: The Hidden Engineers
The human intestinal tract is home to billions of organisms that manage essential transformations the body cannot perform independently. Among these microbial talents is the reduction of bilirubin into urobilino-gen. When gut flora are healthy and diverse, the conversion proceeds smoothly. When they are suppressed — through illness or antibiotic use — urobilinogen levels may drop even when the liver and red blood cell systems are functioning normally.
This dependency is what makes urobilinogen an unusual diagnostic tool: it relies on a biological partnership. In contrast to liver enzymes or bilirubin itself, urobilino-gen is the product of cooperation between human cells and microbial metabolism. Any disturbance to either side of this partnership creates measurable shifts in output.
As research continues to illuminate the microbiome’s influence on systemic health, urobilinogen serves as a small but telling reminder of how deeply intertwined these microbial communities are with the body’s metabolic rhythms.
A Second Table: The Urobilinogen Pathway at a Glance
| Stage of Process | Key Action | Resulting Effect |
|---|---|---|
| Red blood cell breakdown | Formation of bilirubin | Provides precursor for intestinal conversion |
| Liver conjugation | Bilirubin becomes water-soluble | Enables biliary excretion |
| Intestinal bacterial reduction | Bilirubin → urobilinogen | Produces the colorless intermediate |
| Fecal oxidation | Urobilinogen → brown pigments | Colors stool |
| Reabsorption and renal excretion | Portion enters bloodstream and is filtered | Produces trace urinary urobilinogen |
This workflow underscores the compound’s position as a biochemical midpoint, connecting upstream and downstream processes.
Analytical Limits: What Urobilinogen Cannot Reveal
Despite its interpretive value, urobilinogen carries significant limitations. Standard dipstick methods can oxidize quickly or react with unrelated compounds, producing false positives or negatives. Hydration, kidney function, and specimen handling can alter readings independent of disease.
Another constraint lies in its variability. Normal levels can differ widely between individuals, laboratories, and testing methodologies. Without context — bilirubin levels, liver enzyme results, imaging findings, and clinical symptoms — urobilinogen’s alone provides an incomplete picture.
The compound is, in essence, a messenger. It speaks to imbalances in a system but does not specify their location or cause. Its meaning emerges only when interpreted alongside other biochemical and physiological clues.
Evolving Research and Future Possibilities
Although urobilinogen is a longstanding component of routine urinalysis, scientific attention has begun shifting toward its more nuanced implications. With rising interest in the microbiome, the compound now stands at the intersection of liver science, gut ecology, and metabolic research.
Future diagnostic tools may refine how urobilinogen is quantified, distinguish between its intermediates, or map fluctuations more precisely across the enterohepatic cycle. This could transform the compound from a broad indicator into a more sensitive early-warning marker for liver stress, hemolysis, or microbial imbalance.
While such innovations remain in development, the longstanding clinical respect for urobilinogen persists because it reveals something essential: the human body’s most important signals are often hidden not in dramatic biomarkers, but in quiet, continuous processes that unfold beneath our awareness.
Takeaways
- Urobilinogen forms in the intestine through bacterial reduction of bilirubin.
- Its levels reflect the health of liver function, bile flow, gut microbiota, and red blood cell turnover.
- High levels may indicate hemolysis or hepatic dysfunction; low levels suggest obstruction or microbial disruption.
- Interpretation requires context and correlation with additional tests.
- As microbiome research advances, urobilinogen is gaining renewed relevance in understanding gut–liver interactions.
- Despite limitations, it remains a cornerstone of basic diagnostic assessment.
Conclusion
Urobilinogen may appear minor in the vast network of human metabolism, but its significance lies in the connections it represents. Produced quietly in the gut, influenced by bacterial communities, shaped by liver performance, and filtered by the kidneys, it reflects the coherence or disruption of multiple physiological systems.
Because it changes early in many disease processes, urobilinogen offers a subtle but valuable signal for clinicians attempting to detect red blood cell over-destruction, liver strain, or bile obstruction before more overt symptoms emerge. Its presence demonstrates that even in an age of advanced imaging and molecular diagnostics, fundamental biochemical pathways remain among our most reliable indicators of health.
Thus, the study of urobilinogen is ultimately the study of the body’s deeper rhythms — how it processes waste, collaborates with microbes, and communicates imbalance through quiet chemical shifts.
FAQs
What is urobilinogen?
A colorless compound produced in the intestines through bacterial reduction of bilirubin.
Why does urine contain urobilinogen?
A portion of intestinal urobilinogen is reabsorbed, enters circulation, and is filtered by the kidneys.
What makes urobilinogen levels rise?
Increased bilirubin load or reduced liver clearance, often associated with hemolysis or hepatic inflammation.
Why would urobilinogen be absent?
Most commonly due to bile duct obstruction or suppression of gut bacteria.
Is urobilinogen a definitive diagnostic marker?
No. It is informative but must be evaluated alongside other clinical tests and findings.
References
- Hoilat, G. J., & others. (2023). Bilirubinuria. In StatPearls [Internet]. National Library of Medicine.
StatPearls describes how conjugated bilirubin is metabolized by intestinal bacteria into urobilinogen, and how most urobilinogen is excreted in the feces while a small fraction is reabsorbed and excreted in urine. NCBI - MedlinePlus. (n.d.). Urobilinogen in urine. U.S. National Library of Medicine.
This patient-oriented summary explains how urobilinogen is produced from bilirubin by intestinal bacteria, outlines normal and abnormal urinary urobilinogen levels, and links abnormal values to liver disease, bile duct obstruction, or hemolytic conditions. MedlinePlus - StatPearls. (n.d.). Physiology, Bilirubin. In NCBI Bookshelf.
Provides a detailed description of how conjugated bilirubin undergoes bacterial reduction in the colon to produce urobilinogen and stercobilinogen, and explains the roles these compounds play in normal metabolism and pigment formation. NCBI - Sciencedirect Topics. (n.d.). Urobilinogen.
Summarizes urobilinogen’s origin as a bilirubin breakdown product, its reabsorption and excretion via the kidneys, and the way its urinary excretion changes in hemolysis, liver disease, or biliary obstruction. ScienceDirect+2ScienceDirect+2 - TeachMePhysiology. (n.d.). Bilirubin Metabolism.
Describes the pathway from heme breakdown and bilirubin formation to conjugation in the liver, biliary secretion, and eventual microbial conversion to urobilinogen in the intestine. TeachMePhysiology - Song, C., & Liu, Y. (2023). A high urinary urobilinogen / serum total bilirubin ratio indicates acute hepatic porphyria in patients with abdominal pain. Scientific Reports, 13, 21330. https://doi.org/10.1038/s41598-023-48824-9
Presents data showing that urinary urobilinogen levels — when interpreted relative to serum bilirubin — may help diagnose complex conditions like acute hepatic porphyria, illustrating clinical nuance and limitations of standard urinalysis. PMC+1 - Z. A. Kipp et al. (2025). Bilirubin Hepatic and Intestinal Transport and Catabolism. Antioxidants, 14(11), 1326. https://doi.org/10.3390/antiox14111326
This review article outlines modern understanding of bilirubin and urobilinogen metabolism, including gut microbial conversion and enterohepatic cycling, and explores emerging links between these pathways and metabolic or cardiovascular disease