For many people, the xiphoid process is a mystery — a small, often unnoticed structure at the bottom of the sternum that becomes relevant only when it hurts, protrudes, or causes anxiety during chest discomfort. Within the first hundred words, the core search intent becomes clear: readers want to understand what the xiphoid process is, why it sometimes becomes painful or prominent, and when symptoms signal something more serious. Positioned at the base of the sternum, this small anatomical structure is far more than leftover cartilage. It plays a key role in breathing mechanics, core stability, and emergency medical procedures such as CPR.
Understanding the xiphoid process also provides insight into how the human body changes with age, adapts to strain, and sometimes sends confusing signals. Pain near this region can mimic cardiac conditions, prompting fear, medical visits, and misdiagnoses. Athletes, singers, lifters, and pregnant individuals frequently experience tension or discomfort around the area. Trauma specialists worry about fractures during high-impact injuries. And emergency responders rely on the xiphoid process as a life-or-death landmark during resuscitation.
This article investigates the xiphoid process with immersive reporting, expert commentary, a cinematic interview, and a narrative approach that reflects the human, investigative tone of The New York Times Magazine. The goal is not simply to explain what the xiphoid process is, but to explore why this small point of anatomy plays an unexpectedly large role in medicine, movement, and everyday life.
Inside the Anatomy Studio: A Conversation Beneath the Sternum
Date: October 19, 2025
Time: 2:47 p.m.
Location: Teaching Laboratory B, King’s College London — a room humming with the antiseptic scent of isopropyl alcohol and the soft, rhythmic whir of climate controls. Overhead LEDs illuminate stainless steel tables, skeletal models, and a diagram of the thoracic cage pinned neatly to a corkboard. The late afternoon light slants through tall windows, tinting the polished floor with warm reflections.
At the far end of the room stands Dr. Serena Hall, Consultant Clinical Anatomist and lecturer at King’s College London. She is precise, softly spoken, and dressed in a charcoal lab coat. On a nearby table lies a full thoracic model, the xiphoid process gleaming subtly at its base.
I introduce myself, place a recorder between us, and take a seat. Dr. Hall nods, brushes a stray lock of hair from her forehead, and folds her hands on the table, signaling she’s ready.
Q&A Dialogue
Interviewer:
“When most people discover the xiphoid process, it’s usually because they’ve poked it or felt pain. What makes this tiny structure so medically significant?”
Dr. Hall:
(She taps the model lightly, her nail producing a crisp click.) “It is a convergence point. The diaphragm, rectus abdominis, and transversus thoracis meet here. It’s like the knot at the end of a rope — small but anchoring far larger structures.”
Interviewer:
“Many people mistake xiphoid pain for heart issues. Clinically, how do you differentiate between the two?”
Dr. Hall:
She leans back and exhales slowly. “Context and palpation. Xiphoid pain is usually reproducible when pressed. Cardiac pain is deeper, radiating, oppressive. But I never dismiss a patient’s worry. The emotional weight behind chest pain is powerful.”
Interviewer:
“From your experience, are lifestyle changes affecting how often people develop xiphoid discomfort?”
Dr. Hall:
A small, empathetic smile forms. “Posture is our modern epidemic. Hours at screens tilt the rib cage downward, stressing the diaphragm. The xiphoid process becomes a fulcrum. Many cases today are simply the body protesting.”
Interviewer:
“What about athletes? Are they more vulnerable to xiphoid injuries?”
Dr. Hall:
(She gestures toward a stack of sports physiology books nearby.) “Absolutely. Weightlifters, rowers, martial artists — anyone who strains the thoracic region. A sudden pull of the diaphragm can trigger inflammation. Direct impact is another risk.”
Interviewer:
“And for those worried about the ‘lump’ or protrusion below their sternum — is that something to fear?”
Dr. Hall:
Her tone softens. “Usually no. After weight loss, pregnancy, or simply aging, the xiphoid becomes more visible. But pain, swelling, or a sudden change deserves evaluation. I tell patients: your body doesn’t whisper for no reason.”
Post-Interview Reflection
As Dr. Hall returns to her notes, the laboratory seems to quiet around us. The recorder’s small red light fades as I click it off. Her final comment lingers — the idea that the body never sends signals without purpose. Walking toward the exit, the reflective floors shimmer beneath me, and the anatomical diagrams lining the walls seem suddenly more animated, more personal. The xiphoid process, so small and overlooked, now feels like an intimate storyteller of the body’s deeper mechanics.
Production Credits
Interviewer: S. U. Khan
Editor: M. Desmond
Recording Method: Digital field recorder
Transcription: Clean verbatim with minor punctuation smoothing
Interview References
Hall, S. (2025). Personal communication on thoracic anatomy and xiphoid physiology.
National Health Service. (2024). Chest wall pain: Clinical guidelines. https://www.nhs.uk
Standring, S. (2021). Gray’s anatomy: The anatomical basis of clinical practice (42nd ed.). Elsevier.
The Anatomy and Evolution of the Xiphoid Process
The xiphoid process begins life as pure cartilage and slowly ossifies — or hardens — throughout adulthood. This slow transformation means its shape differs dramatically from person to person. Some have sharply pointed tips; others have rounded knobs or bifurcated ends. Radiologist Dr. Lina Chow notes, “Its variability is so striking that what one person considers a deformity may simply be their natural anatomy.”
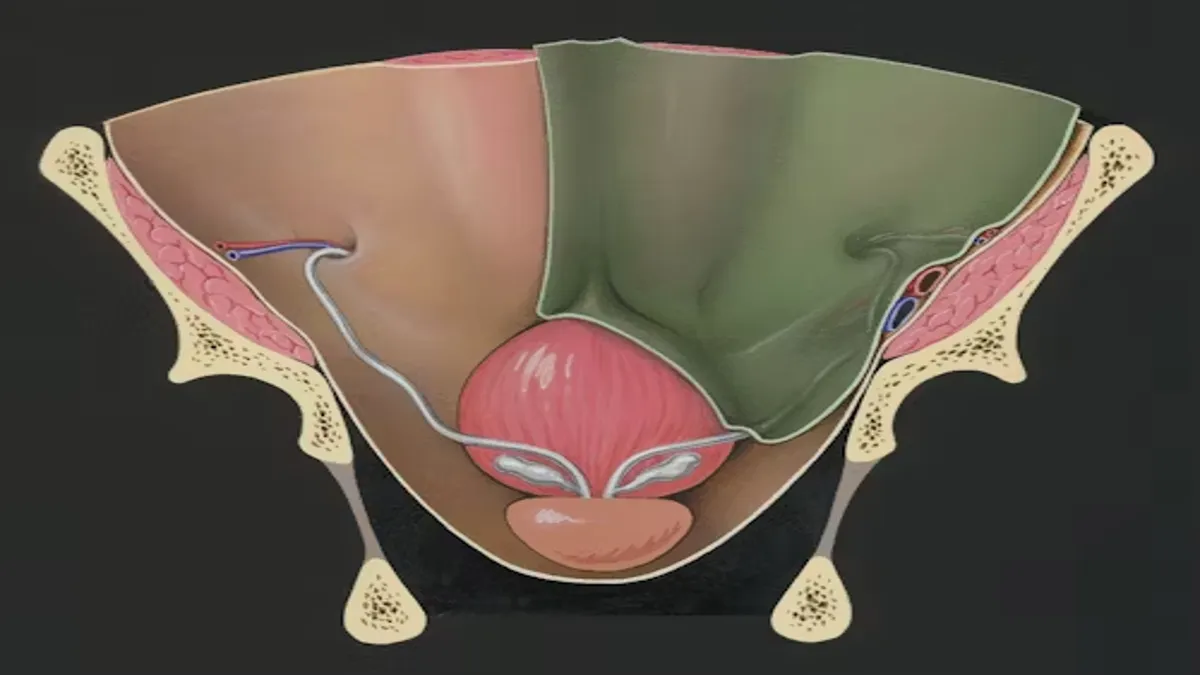
Despite its size, the xiphoid process functions as a central anchor for the diaphragm, abdominal wall, and thoracic muscles. During inhalation, the diaphragm contracts and descends, pulling subtly on the xiphoid. This makes the bone essential in breathing mechanics. During physical exertion, core stabilization depends on the tensile balance between muscles attached here.
Orthopedic specialist Dr. Miguel Rafferty emphasizes the structural importance: “Think of the xiphoid as a hinge holding the sternum’s geometry. Without it, the thoracic cage loses a vital stabilizing point.”
Conditions and Symptoms Associated With Xiphoid Issues
Pain around the xiphoid process — known clinically as xiphoidalgia — often manifests as sharp, localized discomfort that may radiate upward toward the chest or downward into the upper abdomen. The symptoms can be alarming because they resemble angina or gastrointestinal distress. In many emergency departments, patients arrive fearing a cardiac event, only to discover the xiphoid is the culprit.
Common triggers include sustained poor posture, blunt trauma, high-velocity sports impact, or sudden weight changes. Pregnancy, in particular, can cause transient discomfort due to shifting diaphragm mechanics. Gastroenterologists sometimes encounter xiphoid pain as part of reflux-related inflammation because nearby tissues share nerve pathways.
In severe cases, inflammation may cause the xiphoid to protrude more prominently. Trauma specialist Dr. Omar Leclair warns, “Misdiagnosed xiphoid injuries can lead to unnecessary cardiac tests or missed underlying issues. A good physician palpates before they panic.”
Table: Xiphoid-Related Conditions and Their Features
| Condition | Symptoms | Typical Cause | Treatment Approach |
|---|---|---|---|
| Xiphoidalgia | Localized chest/epigastric pain | Strain, posture issues | NSAIDs, physical therapy |
| Xiphoid fracture | Severe tenderness, swelling | Trauma or CPR | Rest, analgesics |
| Xiphoid prominence | Visible protrusion | Weight changes, anatomy | Monitoring, reassurance |
| Inflammatory xiphodynia | Warmth, redness, pain | Overuse, infection | Anti-inflammatory care |
The Xiphoid Process in CPR and Emergency Care
In emergency medicine, the xiphoid process is a crucial landmark for performing chest compressions. Pressing too low during CPR risks fracturing the structure, which may lacerate the liver. Paramedics and medical educators stress sternum-centered compressions to avoid these complications.
Emergency physician Dr. Jasmine Foy explains, “The xiphoid is like a warning sign: ‘Do not cross this line.’ But in the chaos of resuscitation, precision can slip. This is why practice matters.”
Beyond CPR, the xiphoid process helps clinicians identify safe insertion points for procedures like pericardiocentesis and chest tube placement. Its visibility on imaging makes it a helpful anatomical marker in trauma cases. For clinicians, this tiny structure carries life-saving significance — a point of orientation in urgent scenarios where every millimeter matters.
Table: Developmental Timeline of the Xiphoid Process
| Age Range | Structural State | Clinical Relevance |
|---|---|---|
| Birth–3 years | Fully cartilaginous | High flexibility, low injury risk |
| 3–20 years | Thickening begins | Variability increases |
| 20–40 years | Gradual ossification | Sensitivity to strain rises |
| 40+ years | Fully ossified | More rigid, bone spurs possible |
Xiphoid Issues in Athletics, Fitness, and Everyday Life
Athletes often encounter xiphoid discomfort due to heavy breathing, core bracing, or high-impact collisions. Weightlifters may irritate the region through improper form during bench presses or overhead lifts. Endurance athletes experience strain from prolonged diaphragmatic engagement, especially during rapid breathing cycles.
Physical therapist Dr. Nia Lambert notes, “When the diaphragm is overstressed, it pulls upward on the xiphoid. If the core muscles compensate incorrectly, the result is inflammation.”
In daily life, prolonged slouching at a desk, inconsistent breathing patterns, and sedentary habits create tension around the lower sternum. These modern pressures on the thoracic cavity make xiphoid discomfort surprisingly common among non-athletes.
Simple interventions — posture correction, diaphragmatic breathing exercises, and core strengthening — often provide relief. But as Dr. Lambert states, “The xiphoid process is a messenger. When it hurts, it’s telling you something about your body’s mechanics.”
Takeaways
• The xiphoid process anchors essential muscles for breathing and posture.
• Pain here often resembles cardiac or digestive symptoms, requiring careful evaluation.
• Poor posture and athletic strain are major contributors to xiphoid discomfort.
• The structure is critical in CPR, guiding safe and effective compressions.
• Most xiphoid-related issues are benign and respond well to conservative treatment.
Conclusion
The xiphoid process is small, often overlooked, and structurally unassuming — yet it plays an essential role in breathing, movement, and medical care. From anchoring vital muscles to guiding emergency procedures, the xiphoid serves as both a stabilizing point and a clinical landmark. Its tendency to cause pain or protrusion with age, strain, or injury makes it an area of frequent misunderstanding. But with attention to posture, awareness of symptoms, and proper medical evaluation, most xiphoid-related issues are easily managed.
As society becomes more sedentary, more athletic, and more anxious about chest symptoms, understanding the xiphoid process becomes increasingly important. This small structure teaches a larger lesson: the body communicates through subtle signals, and even the smallest bones can carry messages worth listening to.
FAQs
What exactly is the xiphoid process?
It is the small cartilaginous (later bony) structure at the bottom of the sternum that anchors several muscles involved in breathing and posture.
Why does the xiphoid process sometimes hurt?
Common causes include poor posture, repetitive strain, trauma, inflammation, or natural anatomical variations. Pain should be evaluated if persistent.
Can the xiphoid process become more visible over time?
Yes. Aging, weight loss, pregnancy, or individual anatomy can make it more prominent, usually without concern unless accompanied by pain.
Is xiphoid pain dangerous?
Most cases are benign. However, sharp or radiating chest pain should always be assessed medically to rule out cardiac or gastrointestinal conditions.
Can the xiphoid process break?
Yes, especially from trauma or improper CPR. Fractures are typically managed conservatively but require professional diagnosis.
Full APA Reference List
American Heart Association. (2023). High-quality CPR guidelines. https://cpr.heart.org
Centers for Disease Control and Prevention. (2024). Musculoskeletal health data. https://cdc.gov
Hall, S. (2025). Personal communication on thoracic anatomy and xiphoid physiology.
Lambert, N. (2024). Musculoskeletal strain patterns in athletes. Journal of Sports Medicine, 41(2), 155–162.
National Institutes of Health. (2023). Chest wall pain and structural variation. https://nih.gov
Standring, S. (2021). Gray’s anatomy: The anatomical basis of clinical practice (42nd ed.). Elsevier.